As the pandemic enters its fourth year, it remains especially important for older adults who are most at risk for severe illness and death from COVID-19 to remain informed about the latest developments with the disease including new variants and treatments. Here’s a summary of recent coronavirus news that’s particularly relevant to people 50 and older, followed by answers to some of the most frequently asked questions about COVID-19.
Latest COVID-19 news
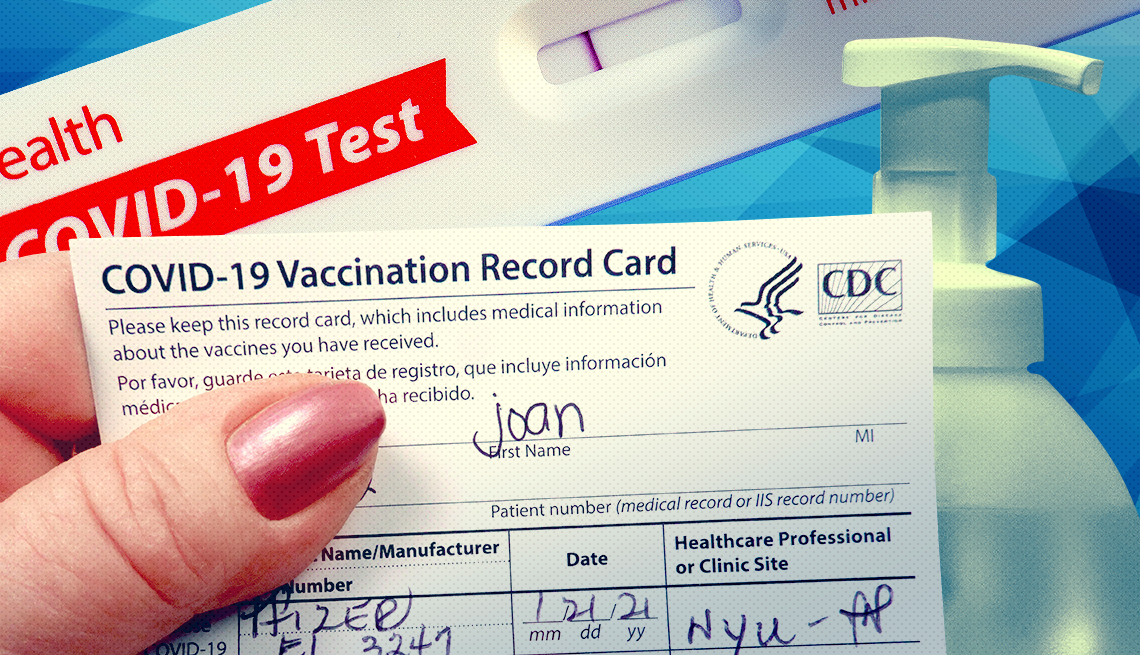
CDC launches bridge program for vaccines (July 14). The Centers for Disease Control and Prevention (CDC) announced plans to launch a bridge program that offers free COVID-19 vaccines to uninsured and underinsured Americans when the vaccines move to the commercial market this fall. When that happens, the agency says COVID vaccines will still be free for most Americans through their health insurance plans. “However, there are 25-30 million adults (ages 18-64) without insurance and additional adults whose insurance will not provide free COVID-19 vaccines after these products move onto the commercial market,” the CDC reports on its website. Under the new bridge program, the agency will purchase COVID-19 vaccines and distribute them to federally qualified health centers and participating pharmacies. Free vaccines through this program will not be available after December 2024.

FDA advisors vote in favor of updating COVID-19 vaccines (June 16). An advisory committee to the U.S. Food and Drug Administration (FDA) voted unanimously on June 15 to update the COVID-19 vaccines to better match the coronavirus strains that are currently circulating in the U.S., most likely taking aim at XBB.1.5, which is part of the omicron family. The XBB.1.5 strain currently accounts for about 40 percent of coronavirus infections in the U.S., federal data shows. Another XBB strain, XBB.1.16, is behind 18 percent of COVID-19 cases in the U.S. If the FDA agrees with its committee’s recommendation, the updated COVID vaccines could be available this fall.
Paxlovid gets full FDA approval (May 25). The oral antiviral pill Paxlovid received full approval from the FDA on May 25 for the treatment of mild to moderate COVID-19. The prescription medication, from drugmaker Pfizer, was first made available under emergency-use authorization in December 2021. It’s recommended for people at high risk of severe illness from a coronavirus infection, including older adults and individuals with underlying health conditions.
Johnson & Johnson vaccine no longer available (May 17). The Janssen (Johnson & Johnson) COVID-19 vaccine is no longer available in the United States. According to the CDC, the government supply of that coronavirus vaccine expired on May 7. The agency has told providers to dispose of any stock they have of that vaccine. The CDC is also advising Americans 18 years old and older who have been vaccinated with the J&J product to now get a dose of the bivalent vaccine — either the Pfizer or the Moderna product. The J&J vaccine has been the least used of the coronavirus vaccines available in the U.S. According to CDC data, of the more than 270 million Americans who have received a coronavirus vaccine, 19 million got the J&J product.
COVID is fourth-leading cause of death for 2022 (May 5). The three leading causes of death for Americans during 2022 were heart disease, cancer and unintentional injury, new provisional data from the Centers for Disease Control and Prevention (CDC) shows. COVID-19, which was the third-leading cause of death in both 2020 and 2021, trailed behind in fourth due to “the large decrease in COVID-19–associated deaths,” the report’s authors write. More than 1.1 million Americans have died from COVID-19 since the start of the pandemic in 2020, and more than 90 percent of deaths have been among people 50 and older.
Health officials support second updated booster (April 19). U.S. health officials have given the green light for people age 65 and older and those with compromised immune systems to receive a second bivalent vaccine. Older adults are now eligible to get a second booster at least four months after receiving their first omicron-specific shot. People with weakened immune systems are eligible for a second booster two months after their initial one. And after that, those with severely compromised immune systems are eligible for additional boosters at their health care provider’s discretion. The additional boosters continue to be free of charge. Health officials have also decided to retire the original Pfizer-BioNTech and Moderna monovalent mRNA vaccines in favor of the updated formula used to target omicron subvariants as well as the original coronavirus.




